A car accident can cause chronic migraines, even if your head wasn’t hit. These may last weeks or become permanent if nerve or spinal damage occurred. In Florida, where crash-related injuries are common, prompt evaluation, diagnosis, treatment, and legal support are key.

From legal rights to medical recovery, this guide walks you through the real causes of chronic migraines after a crash, and what you can do to reclaim your health and future.
Quick Facts: Migraines After a Car Accident
- No head impact needed : whiplash alone can trigger chronic migraines
- Symptoms may be delayed : pain often starts days after the crash
- ER scans often miss the cause : cervical injuries or nerve compression are overlooked
- 14-Day Rule matters : you must seek treatment quickly to qualify for PIP benefits in Florida
- Not just in your head : real injuries can hide behind normal test results
How Can a Car Accident Really Cause Chronic Migraines?
For many crash victims, chronic migraines are puzzling. Especially when the impact seemed “minor,” or there was no direct head trauma. But modern science has shown that your brain doesn’t need to be struck to suffer the consequences of a collision.
Whiplash and Cervical Injury: The Chain Reaction
When a vehicle stops suddenly, even at 15 to 20 mph, the force can whip your neck back and forth violently. That motion stretches and compresses nerves, muscles, and joints in the cervical spine. In many cases, this triggers cervicogenic headaches, which radiate from the neck but feel like traditional migraines: throbbing, one-sided pain, sensitivity to light, even nausea.
Traumatic Brain Injury Without Head Impact
Mild TBIs (traumatic brain injuries) can happen without a direct blow. It’s called a coup-contrecoup injury, where the brain shakes within the skull from the jolt alone. Victims often leave the ER with a “normal” MRI, only to experience weeks or months of migraines, confusion, or fatigue.
That’s because these injuries are often chemical, not structural, causing inflammation or disruption to the brain’s communication pathways. So when patients ask, “I didn’t hit my head, how can I have migraines?”, the answer is: impact isn’t always visible, but the damage is real.
Nerve Compression and Migraine Triggers
One overlooked cause? Pinched occipital nerves. These nerves at the base of the skull can become compressed from swelling or misalignment after a crash. The result is a stabbing, electric pain that mimics classic migraine, but it originates from trauma, not genetics. Sadly, many ERs miss this completely.
The Medical Root Causes Behind Post-Accident Migraines
Post-accident migraines are rarely one-size-fits-all. They emerge from a mix of physical, neurological, and muscular disruptions, and understanding them is key to getting better care and compensation.
Cervicogenic Headaches from Neck Trauma
Whiplash isrupts the delicate alignment between your neck vertebrae, discs, and muscles. This imbalance sends pain signals up the spinal cord to the brainstem, where they manifest as migraines. Yet this source is rarely caught unless cervical spine imaging is ordered.
Occipital Neuralgia: Misdiagnosed and Misunderstood
Occipital neuralgia occurs when the occipital nerves are inflamed or entrapped post-trauma. These nerves can cause migraines that shoot from the neck to the forehead or behind the eyes. Standard migraine treatments won’t touch this pain, it requires nerve blocks or anti-inflammatory therapies. Unfortunately, most emergency care providers overlook this condition altogether.
Migraines from Undiagnosed Mild TBI
Even a so-called “mild” concussion can lead to long-term migraine cycles. Dizziness, light sensitivity, and memory issues may creep in days or weeks later. Without the right tests, many patients are labeled with anxiety or stress, when the issue is neurological.
Muscle Tension and Structural Imbalance
Spinal muscle spasms are another hidden culprit. When upper back or neck muscles go into prolonged contraction (often after a crash), they restrict blood flow and irritate nerves, triggering migraines. In these cases, treatment must go beyond pills, it may involve trigger point injections, chiropractic adjustment, or Botox targeted at muscle groups, not the forehead.
What to Do if Headaches Start Days After the Accident
Many people walk away from a car crash thinking they’re lucky, no cuts, no bruises, just a sore neck. But what happens when a migraine sets in days later?
This delay is more than inconvenient, it can signal deeper, often missed injuries like mild traumatic brain injury, cervical instability, or nerve inflammation. What makes things worse is that this delay also complicates your legal and insurance claims.
Why Delayed Symptoms Matter
Pain that appears 48:72 hours after impact often reflects swelling or nerve compression that’s slowly building pressure. For example, neck muscles that stiffen after trauma can compress the occipital nerves days later, launching a cycle of throbbing headaches. Similarly, post-concussive migraines may not present until inflammation in the brain builds.
The 14-Day Rule in Florida
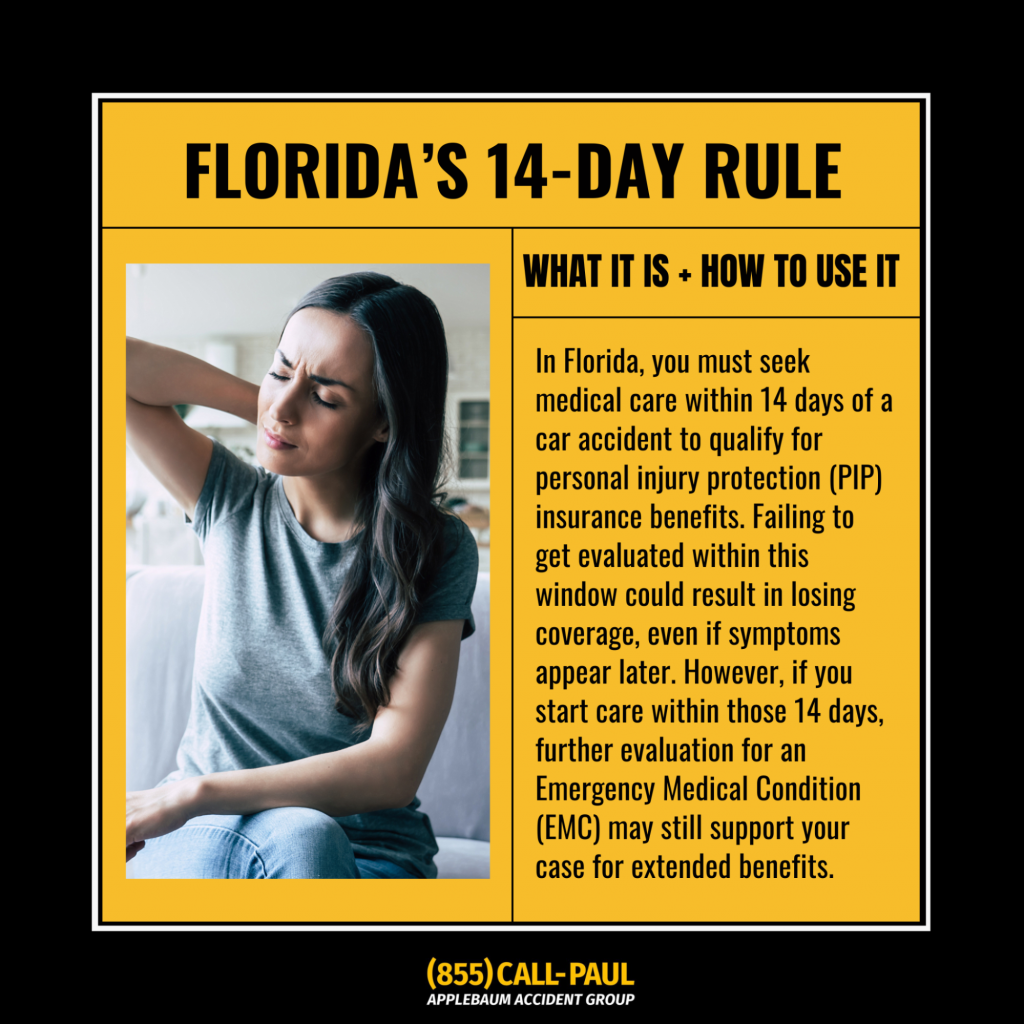
Florida law requires that car accident victims seek initial medical treatment within 14 days to qualify for Personal Injury Protection (PIP) benefits. That means if your migraines appear on day 10 and you wait to act, you could lose access to covered care, even if your condition becomes debilitating later.
This treatment window can directly impact your ability to receive medical and legal support. This guide explains how the Florida 14-Day Accident Law works and what happens if you miss it.
Choose the Right Specialist, Not Just Any Doctor
If you’re asking, “Should I push for a neck MRI or a brain scan?”, you’re asking the right question. Most ERs default to brain MRIs, which may miss spinal issues. But many post-crash migraines originate in the neck, not the skull. In these cases, cervical spine imaging is more revealing.
Your best move: consult with a provider trained in TBI, spine trauma, or post-collision care. Too many patients are discharged with pain meds but no roadmap.
Are These Migraines Temporary or Lifelong?
One of the most painful unknowns for crash survivors is this: “Will I live with this forever?”
The answer depends on the injury source, how quickly you start treatment, and how your body responds, but early warning signs can help predict your outcome.
When Migraines Fade, and When They Don’t
Some headaches fade within a few weeks as the body heals. But when migraines last more than three months, they may become chronic. At that point, your nervous system may have been sensitized, meaning the pain cycle feeds itself.
Red Flags That Signal Long-Term Trouble
- Headaches increase in frequency or severity
- Pain radiates from the base of the skull
- Light sensitivity, balance issues, or blurred vision persist
- No relief from over-the-counter medication
These signs suggest structural or neurological damage. Ignoring them delays healing, and may lock you into a longer-term battle.
Early Intervention Shapes the Outcome
Neurologists and trauma specialists agree: the sooner you start targeted care, the more likely you are to stop chronic migraine development. Waiting too long allows nerve pathways to become hypersensitive, a condition known as central sensitization.
Migraine Treatments That Work for Accident Victims
What helps one patient may do nothing for another, and some treatments can even make things worse if applied too soon or incorrectly.
Physical Therapy: Handle With Care
PT can help, but only when it’s tailored. If the spine is unstable, aggressive manipulation can worsen nerve compression. A focused protocol that considers your imaging results, especially cervical spine MRIs, should come before any stretching or strengthening.
Modern Migraine Tools That Go Beyond Painkillers
Painkillers alone don’t fix chronic post-traumatic migraines. Targeted therapies include:
- CGRP inhibitors (like Ajovy or Emgality): Monthly injections that reduce migraine frequency
- Botox: Reduces muscle tension in the neck and upper shoulders
- Steroid injections: Temporarily reduce inflammation around nerves
- Trigger point therapy: Releases tight knots in overworked muscle groups
Preventative Treatments That Work
Many patients have found success with:
- Ajovy (CGRP inhibitor): Blocks a key molecule involved in migraine inflammation
- Trigger point injections: Interrupt muscular spasm at its source
- Nerve blocks: Target deep structures like the occipital or sphenopalatine nerves
These aren’t quick fixes, but they’re often the breakthrough when first-line treatments fail.
When to Escalate to a Specialist
If you’ve had migraines longer than 6:8 weeks after your crash, it’s time to go beyond general care. Seek out:
- Headache clinics
- Neurologists trained in post-traumatic cases
- Chiropractors specializing in spinal realignment after injury
Does Cervical Alignment Make a Difference?
In many cases, yes. Some patients report significant relief once spinal misalignment is corrected. This doesn’t mean everyone needs chiropractic care, but if imaging shows vertebral compression, alignment can reduce nerve irritation and restore function.
The Legal Side: Can You Sue for Chronic Migraines in Florida?
Many crash victims dealing with chronic migraines feel doubly invisible: their pain isn’t always seen, and their legal rights feel murky. But Florida law allows compensation for both physical and emotional pain after an accident, including headaches that don’t show up on scans.
Florida’s Personal Injury Protections (PIP) and Beyond
Under Florida’s no-fault system, Personal Injury Protection (PIP) covers up to $10,000 in medical bills and lost wages, regardless of who caused the crash. But when migraines become chronic, impact your income, or reduce your quality of life, you may be eligible to pursue a personal injury claim beyond PIP.
This includes damages for:
- Pain and suffering
- Loss of enjoyment of life
- Long-term disability
- Diminished earning capacity
Can you sue for pain and suffering?

Answer: Yes, if your migraines meet Florida’s threshold for serious injury and you have the documentation to back it up. Learn here the Average Car Accident Settlement For Pain And Suffering In Florida.
Why Documentation Is Everything
One of the biggest claim-killers in migraine cases is the lack of medical detail. If you wait too long to get evaluated, don’t see a specialist, or fail to follow up consistently, your case weakens.
Early care does more than support recovery, it’s your paper trail.
Mistakes That Weaken Claims
- Skipping the initial doctor’s visit within the 14-day PIP window
- Relying solely on ER notes (they rarely dig deep enough)
- Failing to document headache frequency, severity, and impact
- Not pushing for cervical spine imaging
When cervical misalignment contributes to migraines, it may factor into your case value: explore how cervical spine injuries like loss of lordosis are evaluated in Florida settlements reading the full article: Loss of Cervical Lordosis Car Accident Settlement Florida.
Real People, Real Pain
While medical journals provide data, real recovery starts with real stories.
- “Doctors didn’t listen until I found my own neurologist.”
- “My insurer said it was just stress, until the MRI showed otherwise.”
- “I didn’t know the neck could be the source until months later.”
What these stories have in common is a delay: in diagnosis, in being believed, in getting help. Every hour wasted made recovery harder.
Lessons They Learned the Hard Way
- Push for cervical spine imaging, not just a brain MRI
- Find a provider who treats post-trauma migraines, not just migraines
- Keep a headache journal to track your symptoms and triggers
- Don’t assume initial “normal scans” mean you’re fine
Don’t Wait, What You Should Do Next

If your headaches started after a car crash, act now, even if they seem manageable today. Waiting risks chronic pain, missed legal deadlines, and irreversible damage.
Seek Medical Care from the Right Specialists
Get evaluated by professionals who understand trauma, not just urgent care doctors. That means:
- Neurologists
- Spine-focused chiropractors
- TBI clinics
- Pain management specialists
Track Your Symptoms Like Evidence
Treat your recovery like a case. Note:
- Migraine frequency and severity
- Triggers and activity limitations
- Missed workdays and lifestyle impact
This log could make the difference in your compensation, and your care plan.
Get Connected with the Right Professionals

At Applebaum Accident Group, we understand the frustration of post-accident migraines, because we’ve helped so many people through it.
If you’re living with pain that doctors can’t explain and insurance won’t acknowledge, you’re not alone. We’ve built a trusted network of attorneys and medical experts across Florida who specialize in cases like yours: A real support system that fights for your recovery, not just your file
👉Contact Applebaum Accident Group today, and we’ll connect you with the people who take your pain seriously, because we do.





